Imagine breathing in tiny, invisible particles every day without even knowing it. For most of us, these microscopic spores pass through our lungs unnoticed, doing no harm. But for some, these same spores are a silent killer, capable of attacking the body from the inside out, slowly rotting tissue and causing organ failure. This is the reality of Aspergillus fumigatus, a deadly airborne fungus that is quietly spreading across the United States.
Unlike the dramatic, world-ending scenarios often depicted in movies or video games, this threat is very real, and it’s here. With rising global temperatures and increasingly humid conditions, the conditions are ripe for this fungus to flourish in the warmest, dampest parts of the country. Florida, Louisiana, Texas, Georgia, and California are seeing the worst of it, but the risk is spreading, especially in areas with aging infrastructure and crowded cities.
What makes this threat so alarming is not just its ability to infect vulnerable individuals, but its potential to evade treatment. As drug-resistant strains of the fungus become more common, medical experts warn that the current response may be inadequate, putting hundreds of thousands of lives at risk. In a world already grappling with the effects of climate change, this silent epidemic may be one of the most underestimated dangers we face.
So, how do we respond to a microscopic invader that can strike without warning? And more importantly, what can we do to protect ourselves and those we care about from a fungus that may be growing in the air we breathe? The time to find answers is now, before it’s too late.
What is Aspergillus Fumigatus?
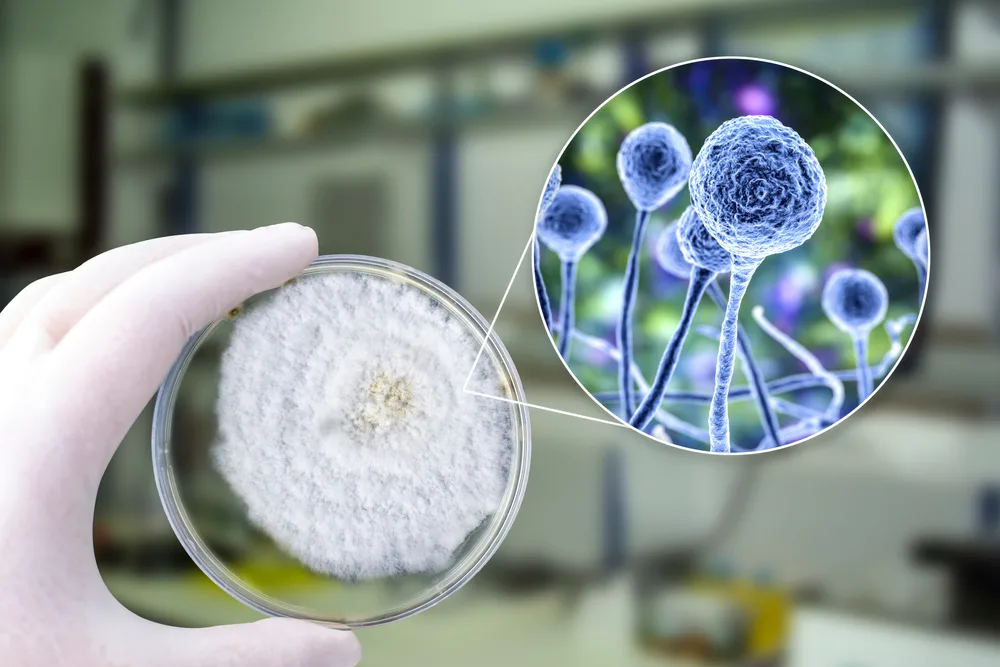
Aspergillus fumigatus is a type of mold that thrives in the environment, invisible to the naked eye but incredibly persistent. Its tiny spores, called conidia, are carried effortlessly by the wind, floating through the air and infiltrating homes, hospitals, and even agricultural fields. These spores are so minuscule that most people breathe them in without even realizing it—every day, potentially without consequence. But for some, these invisible invaders can be deadly.
This fungus is found in soil, decaying plant matter, and even indoor dust, making it nearly impossible to avoid. It thrives in warm, damp conditions, which makes places like compost piles, humidifiers, and poorly ventilated buildings ideal breeding grounds. In fact, Aspergillus fumigatus can survive in temperatures over 120 degrees Fahrenheit, which is why it’s often found in agricultural settings where such conditions are common, especially in places that experience prolonged periods of heat.
For the majority of people with healthy immune systems, the spores cause no harm. The body’s natural defenses fight off the fungus before it can settle in the lungs or other parts of the body. However, for those with weakened immune systems—such as cancer patients, people with HIV, or those recovering from serious infections like influenza—this fungus becomes a serious threat. It can trigger an aggressive infection known as aspergillosis, which can cause devastating damage to the lungs and, in severe cases, spread to other organs such as the brain, heart, and kidneys.
Unlike some infections, aspergillosis doesn’t always show immediate symptoms, which can delay diagnosis and treatment. In many cases, it starts as a chronic condition, where the infection persists and slowly worsens, causing long-term lung damage. For the most vulnerable individuals, invasive aspergillosis can be fatal.
From Lung Infections to Organ Failure

When Aspergillus spores enter the lungs, they can cause a condition called aspergillosis. This infection starts as an inflammation in the lungs, where the fungus infiltrates the airways and tissues, causing symptoms like persistent cough, chest pain, difficulty breathing, and fever. If left untreated, aspergillosis can escalate, leading to chronic pulmonary aspergillosis (CPA). This long-term lung infection can cause scarring, impair lung function, and significantly reduce a person’s quality of life. Around 400,000 cases of CPA occur annually in the U.S., and though it is treatable, it often requires prolonged, intensive care.
Invasive aspergillosis, however, represents a much more severe form of the disease. This rare, but deadly complication occurs when the fungus spreads from the lungs to other vital organs, such as the brain, heart, kidneys, and liver. For individuals with severely weakened immune systems—such as organ transplant recipients, cancer patients undergoing chemotherapy, or those with HIV—the risks are even higher. Invasive aspergillosis is often rapid, aggressive, and difficult to treat, with mortality rates exceeding 50% for those infected.
In one study, only 59% of organ transplant patients survived a year after being infected with invasive aspergillosis, and the survival rate was even lower for stem cell transplant recipients, at just 25%. These numbers highlight the brutal nature of the disease and the urgent need for better detection and treatment methods.
The impact is not just medical—it’s also financial. Hospitalizations for aspergillosis have risen steadily, with an estimated 15,000 cases recorded by 2014. The associated costs are significant, with one study putting the price of treating aspergillosis-related hospitalizations at approximately $1.2 billion annually.
In the most severe cases, aspergillosis can be fatal. It has been ranked among the top four infections likely to cause death in ICU patients, according to autopsies of those who succumbed to the disease. The combination of widespread exposure, delayed diagnosis, and the fungus’s ability to resist treatment in certain cases make it a formidable and often underestimated threat.
Which States and Cities are Affected?
The states facing the highest exposure—Florida, Louisiana, Texas, Georgia, and California—share a common profile: warm, humid climates that create ideal conditions for fungal growth. In these environments, the fungus can thrive in soil, compost piles, decaying vegetation, and even indoor dust. Farming activity further intensifies the problem. Agricultural areas frequently use azole-based fungicides to protect crops, which not only encourage fungal survival in the soil but also drive the development of drug-resistant strains.
Major cities within and beyond these states are also becoming fungal hotspots, particularly those with dense populations and aging infrastructure. Urban centers like New York, Los Angeles, and Houston are examples of areas where the combination of population density, pollution, and deteriorating buildings makes it easier for Aspergillus spores to circulate and take hold. Hospitals in these areas are especially concerned, as construction, water leaks, and poor ventilation can increase the fungal load indoors—putting vulnerable patients at greater risk of infection.
It’s not just outdoor environments that matter. Indoor air quality, particularly in older buildings without proper mold control or filtration, can contribute to the risk. High humidity levels indoors, coupled with inadequate ventilation or neglected maintenance, allow spores to persist and multiply. In health care settings, this becomes a major concern, prompting hospitals in high-risk states to adopt stricter mold inspection protocols and antifungal safeguards.
The regional differences also tie directly into the broader issue of climate change. Warmer temperatures and more frequent extreme weather events—like hurricanes, flooding, and heatwaves—further destabilize ecosystems and expand the territory where Aspergillus fumigatus can thrive. According to projections from the University of Manchester, if fossil fuel use continues at current levels, the range of this fungus could expand by over 75% in the U.S. by the end of the century, placing millions more at risk, especially in the southern states where environmental conditions mirror these forecasts.
The Role of Climate Change in Fungus Spread

Aspergillus fumigatus prefers warm, damp environments. It grows efficiently at human body temperature (around 37°C) and can survive in much hotter conditions, even above 120°F, such as those found in compost piles or overheated agricultural environments. As global temperatures continue to rise, more regions are becoming biologically hospitable to this heat-loving fungus. What was once an issue concentrated in a few southern states may soon become a nationwide concern.
Modeling studies from the University of Manchester provide a chilling projection: under a high-emissions scenario (where fossil fuel use continues at current rates), the geographic range of A. fumigatus could expand by more than 75% in the U.S. by 2100. This would expose millions more people, particularly in the southern and midwestern states, to environments conducive to fungal growth. Europe and Africa are seeing similar shifts. In some parts of Africa, temperatures may become so extreme that certain fungi can no longer survive, while other regions will become fungal hotspots. The implications are global, but in the U.S., the South—with its increasingly long, hot growing seasons and frequent flooding—faces the most immediate risks.
Beyond just temperature, climate change also affects the natural cycles of moisture and wind. More humidity means more fungal growth. More wind and dust storms mean more spores being dispersed into the air, increasing the likelihood of inhalation. Additionally, the aftermath of climate-driven disasters—such as hurricanes or wildfires—can create ideal conditions for fungal outbreaks. Water-damaged buildings, displaced populations, and overwhelmed healthcare systems all contribute to heightened exposure and reduced ability to respond.
There’s also the matter of adaptation. Aspergillus fumigatus is genetically flexible, able to evolve quickly in response to environmental stressors. As climate pressures increase, the fungus is not just surviving—it’s adapting, expanding, and even becoming more resistant to antifungal drugs. This means that climate change isn’t just increasing where the fungus can live; it’s also accelerating its evolution into a more dangerous, harder-to-treat pathogen.
Public health experts have long warned that fungal diseases are an underappreciated consequence of global warming. Dr. Norman van Rhijn, a fungal specialist at the University of Manchester, emphasized that we’ve already seen fungi like Candida auris emerge in response to temperature shifts. Aspergillus fumigatus is now following a similar path—quietly adapting to a world in flux, moving into new territories, and becoming harder to control.
The Growing Threat of Drug Resistance

Azoles, a class of antifungal drugs, are the cornerstone of treatment for aspergillosis. They are used both in clinical settings to treat patients and extensively in agriculture to prevent crop loss. This dual use, however, is creating a perfect storm. Fungicides used in farming—chemically similar to the medical azoles—are promoting the development of resistance in environmental Aspergillus populations. When these resistant spores are inhaled by humans, especially those with weakened immune systems, the infections become much harder to treat and significantly more deadly.
A study published in Applied and Environmental Microbiology found azole-resistant Aspergillus fumigatus strains in farm soil across at least seven U.S. states. In many cases, these resistant strains were no longer responsive to first-line antifungal treatments. Patients infected with drug-resistant strains face a grim prognosis: mortality rates can exceed 50%, and the alternative treatments are often more toxic, affecting organs like the liver and kidneys. In the most vulnerable groups—organ transplant recipients, cancer patients, or those with chronic lung conditions—the treatment window is narrow, and resistance can mean the difference between life and death.
The agricultural connection is particularly troubling because resistance genes can be introduced far from where the infections occur. A person living in a city might never set foot on a farm but can still inhale resistant spores that traveled hundreds of miles on the wind. Public health officials are now tracking resistance markers in soil, compost, and hospital environments to better understand how these genes move and where they are most prevalent.
Hospitals are beginning to take action, with increased surveillance, specialized mold inspections, and stricter antifungal stewardship. But the tools to fight resistant fungal infections are still limited. Unlike the pipeline of antibiotics for bacterial infections, antifungal drug development is sparse. Only a few new classes of antifungal drugs have been introduced in recent decades, and clinical trials often exclude children and other high-risk groups.
The World Health Organization has recognized the seriousness of the threat, listing Aspergillus fumigatus as a “critical priority” pathogen in 2022. It urged immediate investment in safer antifungal drugs, faster diagnostic tools, and improved training for healthcare professionals. Without these interventions, experts warn that resistant Aspergillus could lead to a growing number of untreatable infections—quietly spreading through soil, air, and hospitals alike.
Prevention and Precautionary Measures

Doctors and infectious disease specialists strongly advise immunocompromised individuals to avoid high-exposure environments where fungal spores are more likely to be airborne. These include places like gardens, compost piles, construction sites, and damp or moldy indoor areas. Simple lifestyle adjustments, such as wearing N95 masks in dusty environments, using high-efficiency particulate air (HEPA) filters indoors, and maintaining dry, well-ventilated living spaces, can significantly reduce spore inhalation. Avoiding activities like gardening or yard work—or at least taking proper precautions while doing them—is especially important for patients recovering from chemotherapy, organ transplants, or severe viral infections like COVID-19 or influenza.
In medical settings, the stakes are even higher. Hospitals, particularly those treating immunocompromised patients, have begun ramping up mold inspections and strengthening antifungal protocols. These include measures like regular air filtration checks, sealed patient rooms with controlled airflow, and limiting building construction or renovations near sensitive wards, as construction dust can carry large amounts of fungal spores. Some facilities also preemptively test patients for early signs of fungal infection and monitor environmental spore counts as part of their infection control strategies.
From a broader public health perspective, early detection and rapid treatment are key. However, fungal infections often go undiagnosed until they become severe because symptoms mimic those of bacterial or viral respiratory illnesses. This diagnostic gap underscores the need for investment in faster, more accurate testing methods—tools that could enable clinicians to detect aspergillosis before it becomes invasive and difficult to treat.
Education is another essential tool. Many people are unaware that fungal infections can be as serious as bacterial or viral diseases, or that certain occupations and environments may increase their risk. Public awareness campaigns could help individuals understand how to reduce exposure and recognize early warning signs of fungal infection, such as persistent coughing, shortness of breath, or unexplained fatigue in high-risk individuals.
On the agricultural and policy fronts, revisiting the use of azole-based fungicides is crucial. Striking a better balance between protecting crops and limiting the environmental spread of resistant fungi will require regulatory reform, the development of safer fungicide alternatives, and increased collaboration between the agricultural and healthcare sectors.
The Importance of Monitoring and Research
One of the most pressing challenges in the fight against Aspergillus fumigatus is the lack of comprehensive surveillance and research. Unlike many bacterial or viral infections, fungal diseases often fall through the cracks of public health systems. In the United States, aspergillosis is not a reportable disease, meaning there is no standardized system to track its incidence, hospitalizations, or mortality. This data gap makes it difficult to grasp the full scope of the threat—or to respond effectively as the fungus continues to spread and evolve.
Monitoring efforts are especially critical as antifungal resistance rises. Without widespread environmental and clinical tracking, resistant strains can quietly gain a foothold before they’re detected. Public health experts are now advocating for integrated surveillance systems that monitor not just human infections, but also environmental spore loads in soil, compost, and indoor air, particularly in hospitals and agricultural zones. Such efforts would allow authorities to identify hotspots early, monitor trends in resistance, and target interventions more efficiently.
Research, too, remains vastly underfunded compared to other infectious diseases. Despite the fact that fungi are responsible for an estimated 1.5 to 3.8 million species globally—and that new pathogens are emerging as the climate warms—fungal diseases receive only a fraction of the attention and funding allocated to viral or bacterial threats. This lack of investment has left gaping holes in our understanding. Fewer than 10% of fungal species have been formally described, and even fewer have had their genomes sequenced. Without this foundational knowledge, the development of vaccines, rapid diagnostics, and new antifungal drugs lags behind.
Organizations like the World Health Organization have begun to recognize the urgency. In 2022, WHO released its first-ever priority list for fungal pathogens, placing Aspergillus fumigatus among the highest threats due to its drug resistance, global distribution, and high mortality rates. The agency called for greater funding, international collaboration, and incentives for pharmaceutical companies to develop safer, more effective antifungal treatments.
Experts are also calling for research that looks ahead—using predictive models to anticipate how fungi will spread under various climate scenarios and how different policies might influence resistance patterns. For instance, the MaxENT model used by researchers at the University of Manchester has already shown how A. fumigatus could expand dramatically by the end of the century, threatening millions more people in new regions. This kind of forecasting is invaluable for shaping long-term public health strategies.
Perhaps most crucially, experts urge better cross-disciplinary cooperation. Fungi do not respect human boundaries—they move between agricultural fields, hospital rooms, and natural ecosystems. Effective solutions will require scientists, clinicians, farmers, and policymakers to work together, sharing data and aligning goals.
Why We Should Care

Fungal infections are often underreported and underestimated, yet they cause more than 1.5 million deaths globally each year, rivaling diseases like tuberculosis. And unlike many viruses or bacteria, fungal pathogens are harder to detect, more difficult to treat, and often overlooked in medical training and public health planning. Aspergillus fumigatus is just one of many fungal threats gaining ground as global temperatures rise and ecosystems shift. Others, like Candida auris and Cryptococcus, are also taking advantage of warming climates and weakened immune systems worldwide.
The rise of fungal pathogens is a canary in the coal mine—a quiet signal that environmental disruption is altering the microbial balance in our world. As temperatures increase, new regions become breeding grounds for fungi that were previously contained. At the same time, the overuse of antifungal drugs in agriculture is pushing fungi to evolve resistance faster than our treatments can keep up. It’s a feedback loop: climate change fuels fungal growth, resistant strains thrive, and the margin for medical intervention narrows.
There’s also a food security dimension. Aspergillus species produce aflatoxins—naturally occurring carcinogens that can contaminate crops like corn, peanuts, and grains. A single outbreak can cost the U.S. agricultural industry over $1 billion in losses. Contaminated food supplies don’t just harm economies—they pose real health risks to consumers, especially in regions where food monitoring systems are weaker or underfunded.
What’s perhaps most sobering is that this crisis is largely invisible. Unlike a pandemic that brings society to a halt, fungal threats unfold slowly, often in hospitals, rural fields, or homes with poor ventilation. There are no dramatic headlines or instant spikes in data—just a steady rise in severe infections, treatment failures, and preventable deaths.
A Wake-Up Call for the Future
The rise of Aspergillus fumigatus as a public health threat is not a fluke—it is a clear and pressing signal of the changing world we live in. As temperatures rise, ecosystems shift, and drug resistance accelerates, we are witnessing the conditions that allow an environmental fungus to become a lethal, treatment-resistant pathogen.
This is not just a story about a single fungus. It’s a warning about the cascading consequences of climate change, unchecked agricultural practices, underfunded medical research, and the growing blind spots in public health infrastructure. When fungal infections that were once rare begin to cause widespread illness and death, and when standard treatments begin to fail, we are no longer dealing with isolated incidents—we are facing a systemic risk.
But the future is not fixed. Coordinated action today can blunt the impact of this threat. That means investing in antifungal drug development, updating agricultural policies, improving indoor air quality, tracking fungal infections more rigorously, and educating the public and healthcare workers alike. It also means addressing climate change with the urgency it demands—because the warmer our planet gets, the more favorable the conditions become for pathogens like Aspergillus fumigatus to thrive.
In a world hyper-focused on viruses and bacteria, fungal diseases remain dangerously underestimated. Yet they are growing stronger in silence. This is our opportunity to catch up—to treat the microscopic world with the seriousness it deserves, before a once-manageable fungus evolves into something far more devastating. The window for preparedness is still open, but not indefinitely. Now is the time to act.