You walk into the imaging suite for a routine MRI, expecting clarity—perhaps even peace of mind. But what if, beneath the hum of the machine and the promise of early detection, something else was quietly forming inside your body?
For decades, MRI scans have been a medical marvel—non-invasive, radiation-free, and often crucial in diagnosing everything from brain tumors to spinal injuries. Yet, new research is challenging long-held assumptions about the safety of one key ingredient: the contrast agent used to sharpen those detailed images. Specifically, scientists have found that gadolinium, a rare earth metal used in millions of scans each year, may linger in the body and—in some cases—transform into nanoparticles that embed themselves in human tissue.
The findings are early but significant, pointing not to panic, but to a deeper understanding of how our bodies interact with medical technologies. As researchers peel back the layers of this invisible process, the implications could reshape how we think about contrast-enhanced MRI scans and who might be most at risk.
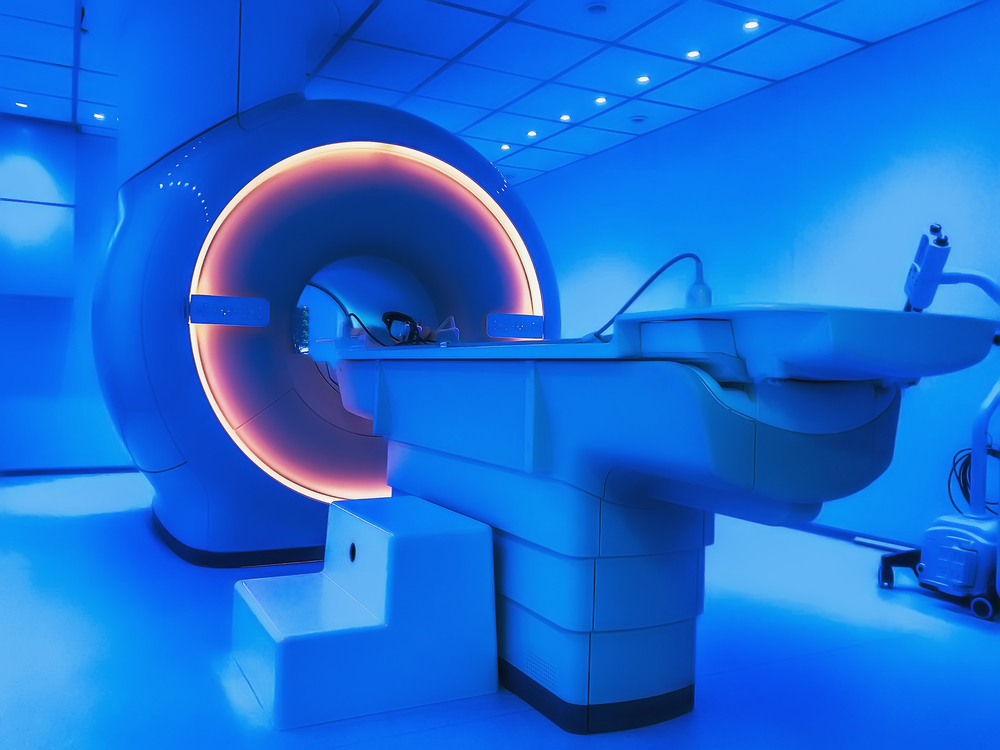
How MRI Scans Work
Magnetic Resonance Imaging, or MRI, has revolutionized diagnostic medicine by offering a highly detailed view inside the human body—without the risks associated with radiation. At the core of this technology is a powerful magnet that interacts with the body’s natural chemistry. Since our tissues are composed largely of water, and water contains hydrogen atoms with magnetic properties, MRIs work by aligning these hydrogen protons using a strong magnetic field. When radiofrequency pulses are applied, the protons are momentarily knocked out of alignment, and as they return to their original state, they emit signals that are captured and converted into high-resolution images.
Unlike X-rays or CT scans, which are better suited for imaging bone, MRIs excel at visualizing soft tissues—like the brain, spinal cord, muscles, and internal organs. This makes MRI indispensable in diagnosing conditions such as multiple sclerosis, tumors, torn ligaments, and vascular abnormalities. Moreover, it’s the preferred imaging method in scenarios requiring repeated scans, particularly for neurological conditions or pediatric care, because it doesn’t expose patients to ionizing radiation.

In many cases, to enhance the diagnostic accuracy of an MRI, a contrast agent is administered intravenously. Gadolinium-based contrast agents (GBCAs) are the most common. These compounds highlight abnormalities by altering the magnetic properties of nearby water molecules, which helps radiologists distinguish between healthy and diseased tissues with far greater precision.
While not all MRI exams require contrast—musculoskeletal scans, for instance, often don’t—contrast-enhanced MRI is often essential in evaluating complex or life-threatening conditions such as cancer, inflammatory diseases, or vascular lesions. “Contrast is only used when it’s necessary,” emphasizes Dr. Richard Reitherman, a radiologist and medical director of breast imaging. “It can be the difference between seeing a subtle tumor or missing it entirely.”
What Researchers Discovered

While gadolinium-based contrast agents (GBCAs) have long been considered safe when used properly, new findings from researchers at the University of New Mexico are challenging that assumption—not by casting doubt on the widespread use of MRIs, but by shedding light on how the body might react under certain, previously overlooked conditions.
The study, published in the journal Magnetic Resonance Imaging, focused on a subtle but potentially significant interaction between gadolinium and a naturally occurring compound called oxalic acid. Found in many common foods like spinach, chocolate, nuts, and berries, oxalic acid is known for its ability to bind with minerals, a process that contributes to kidney stone formation when it binds with calcium. The researchers asked: what happens when it binds with gadolinium?
In a series of controlled lab experiments, the UNM team discovered that oxalic acid can trigger gadolinium—normally tightly bound within contrast agents—to break free and reassemble into nanoparticles. These tiny particles are small enough to infiltrate cells in critical organs such as the kidneys, brain, and liver. Importantly, this transformation was observed outside the human body, in test tube models, but it raised an urgent biological question: if this can happen in vitro, could it happen in vivo—within patients—especially those with high oxalate levels due to diet, supplements, or underlying metabolic conditions?
Dr. Brent Wagner, the study’s senior author and a professor of internal medicine at UNM, believes the answer may explain a longstanding medical mystery. Some patients have developed severe complications, including nephrogenic systemic fibrosis (NSF), after just a single gadolinium-enhanced MRI. “This nanoparticle formation might explain why there’s such an amplification of the disease,” Wagner said. “When a cell is trying to deal with this alien metallic nanoparticle within it, it’s going to send out signals that tell the body to respond to it.”
The idea is that once gadolinium escapes its molecular “wrapper,” it becomes biologically reactive again—potentially toxic and capable of triggerin
g an inflammatory or fibrotic response. The researchers suspect that metabolic differences among individuals—especially those with higher oxalate levels—could determine who is vulnerable. This might explain why most people tolerate GBCAs without issue, while a small subset experiences serious, even life-altering, side effects.
Who Is at Risk

While the recent findings on gadolinium nanoparticles have understandably raised concern, medical experts are urging caution in interpretation—not in the use of MRI itself. The vast majority of patients who undergo contrast-enhanced MRI scans experience no adverse effects. For most, gadolinium is efficiently processed and excreted from the body, typically through the kidneys, with no lingering complications.
However, a small subset of patients may be at higher risk. Chief among them are individuals with chronic kidney disease or impaired renal function, who cannot efficiently clear gadolinium from their system. In these cases, the metal may remain in circulation longer, potentially increasing the likelihood of tissue deposition and inflammatory reactions. These patients have been shown to be more susceptible to nephrogenic systemic fibrosis (NSF), a rare but serious condition characterized by thickening and tightening of the skin and connective tissues, sometimes affecting internal organs.
What the new research adds is a potential metabolic dimension to that risk profile. According to Dr. Brent Wagner and his team, individuals with elevated oxalic acid levels—due either to diet, vitamin C supplements, or specific metabolic conditions—might be more prone to nanoparticle formation. This could explain why some people have significant reactions to gadolinium after only one exposure, while others tolerate multiple scans without issue.
Yet, even among those with detectable gadolinium accumulation—in organs such as the brain or kidneys—there is currently no conclusive evidence linking these deposits to symptoms or disease in the general population. “Although gadolinium is generally considered to be safe when used as directed, it is associated with adverse effects in certain patient populations,” said Dr. Kelly Johnson-Arbor, a toxicologist at MedStar Health. Importantly, serious complications remain extremely rare. One study estimates that they occur in just 0.03% of gadolinium-based contrast injections.
It’s also worth distinguishing this concern from heavy metal poisoning, a term that can often spark unnecessary fear. While gadolinium is a metal, its presence in the body—especially in nanoparticle form—has not yet been shown to mimic the effects of toxic metals like lead or mercury. As Dr. Jeffrey Luci, a biomedical imaging expert at Rutgers University, puts it: “No one has been able to show that gadolinium is doing anything bad. But that doesn’t mean we shouldn’t be looking for reasons to make sure it’s safe.”
Medical Implications

One of the most promising developments is the creation of an international patient registry spearheaded by Dr. Brent Wagner’s team at the University of New Mexico. This initiative is designed to systematically gather biological samples—blood, urine, hair, and fingernails—from individuals who report symptoms after gadolinium exposure. The goal is to uncover patterns that could help identify those at greater risk for complications. By correlating these biological markers with medical history, medication use, and dietary habits, researchers hope to build a clearer picture of who is susceptible to adverse reactions and why.
This kind of precision profiling represents a potential turning point. In the future, patients may be screened for high oxalate levels or genetic markers that predispose them to complications, enabling physicians to tailor imaging plans accordingly. In some cases, alternative imaging methods could be explored, or non-gadolinium contrast agents might be used. In others, small behavioral modifications—such as avoiding vitamin C supplements before a scan—could help minimize risk, particularly if future studies confirm that such factors influence nanoparticle formation.
The findings could also influence how contrast agents are formulated. Most current gadolinium-based agents are designed to tightly bind the metal and allow for swift excretion. However, this research may push manufacturers to develop next-generation compounds that are even more stable or less reactive to compounds like oxalic acid in the body.
At a broader level, this study underscores the need for more translational research—bridging the gap between lab discoveries and clinical practice. As experts have noted, the current conclusions are based on in vitro (test tube) experiments, and more work is needed to establish whether these nanoparticles form and behave similarly inside the human body. “This is the basic science, and it’s where we start,” said Dr. Reitherman. “But it needs to move on to human experimentation and prove that this actually causes disease.”
Balancing Innovation with Caution

Dr. Jamie Alan, associate professor of pharmacology and toxicology at Michigan State University, emphasizes that this is preliminary science. “This was not done in humans and may not translate,” she notes. “We really need more research to completely understand the long-term health effects and potential treatments.” Her point reflects a common refrain among professionals: findings in controlled laboratory environments often behave differently in the complexity of the human body.
Radiologist Dr. Richard Reitherman echoes this cautious optimism. Gadolinium, he explains, is not used indiscriminately—it is administered only when it offers clear diagnostic benefits. “Contrast is used for a lot of things and millions of people have had millions of doses of this with no issue,” he says. For conditions such as brain tumors, breast lesions, or suspected cancers, contrast-enhanced MRIs often offer the clearest, most accurate diagnosis available. In such cases, the information gained far outweighs the potential for long-term harm.
Dr. Jeffrey Luci, a biomedical researcher at Rutgers University, adds that accumulation of gadolinium in the body has not yet been definitively linked to disease. While it’s true that traces of the metal can remain in organs like the brain and kidneys years after exposure, Luci warns against jumping to conclusions. “No one has been able to show that gadolinium is doing anything bad,” he says. “But that doesn’t mean we shouldn’t be looking.”
It’s a sentiment that strikes the right balance between vigilance and reassurance. Gadolinium’s risks are not being ignored; they are being examined more closely than ever before. Toxicologists like Dr. Kelly Johnson-Arbor support this shift, particularly for vulnerable groups such as patients with kidney disease or those with specific metabolic conditions. For these individuals, individualized risk assessments may become a new standard of care as the science evolves.
What experts agree on most is that patients should never feel discouraged from seeking care. If a physician recommends an MRI with contrast, it’s because the potential insights it provides are critical to diagnosis or treatment planning. As Dr. Alan reminds patients, “Generally, this imaging is safe. Serious adverse reactions are rare.”
Informed, Not Alarmed
The evolving research around gadolinium and MRI contrast agents serves as a timely reminder of the delicate balance between medical innovation and patient safety. It is not a call for fear, but a call for awareness—particularly as science uncovers more about how individual biology and lifestyle may influence our reactions to even the most routine procedures.
MRI technology remains one of the most powerful diagnostic tools in modern medicine. It has saved lives, advanced early detection, and offered peace of mind to millions. Gadolinium-based contrast agents, when used appropriately, have helped illuminate hard-to-detect conditions ranging from cancer to neurological disorders. For the overwhelming majority of patients, the benefits continue to far outweigh the risks.
Yet, as we’ve seen from the recent findings, the medical community is not standing still. Scientists, radiologists, and toxicologists are asking better questions—about metabolism, diet, long-term accumulation, and individual susceptibility. These questions are not only valid; they’re vital. They open the door to more personalized, informed care and to potential safeguards that could make this life-saving technology even safer.
For patients, the best course of action is to stay informed and communicate openly with healthcare providers. If you have kidney disease, take supplements like vitamin C, or have concerns about prior gadolinium exposure, talk to your doctor. Together, you can weigh the benefits and risks and make decisions grounded in both science and your specific health needs.
In medicine, progress often begins with questions. The recent research is just that—a beginning. And it’s a promising one.



Reba Boyle
Sunday 11th of May 2025
Doğayı seven, kuşları tanımak isteyen veya üretim konusunda kendini geliştirmek isteyen herkes için serinofil.com bir başvuru kaynağı niteliğinde.