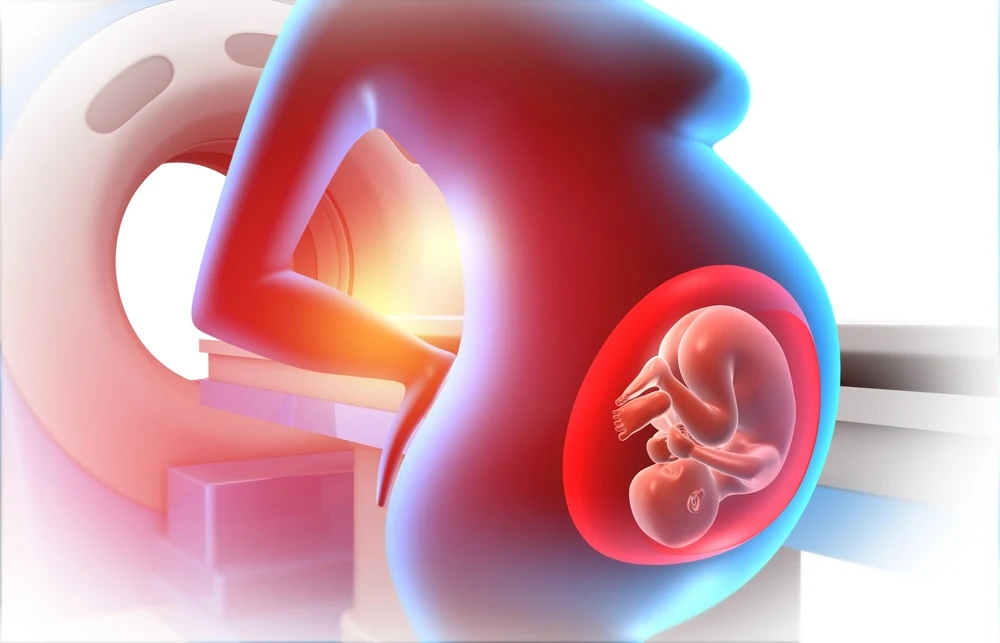
The federal government has officially removed the COVID-19 vaccine from the CDC’s recommended immunization schedule for healthy children and pregnant women. This marks a major reversal from earlier public health guidance that encouraged widespread vaccination across all age groups. Announced by Health and Human Services Secretary Robert F. Kennedy Jr., along with top officials from the NIH and FDA, the change reflects updated scientific data, shifting international norms, and growing concerns about the risk-benefit balance for low-risk populations. The updated guidance applies only to individuals without underlying health conditions and does not affect access to the vaccine for those who remain eligible or choose to receive it.
The announcement comes amid growing calls for a more evidence-based approach to pandemic-era policies. Many experts and parents have questioned the need for repeated COVID shots in children and healthy pregnant women, especially as hospitalization and death rates in these groups remain low. With this move, federal agencies are signaling a pivot toward individualized risk assessments and away from universal mandates.

DC Drops COVID Vaccine Recommendation for Healthy Kids and Pregnant Women
In a major shift in federal public health policy, the COVID-19 vaccine is no longer recommended on the CDC’s immunization schedule for healthy children and pregnant women. The announcement was made by Health and Human Services Secretary Robert F. Kennedy Jr., alongside NIH Director Dr. Jay Bhattacharya and FDA Commissioner Dr. Marty Makary. This change reverses the Biden administration’s previous stance, which had promoted widespread vaccination in these low-risk groups. The updated recommendation excludes only those without underlying health conditions and does not restrict access for higher-risk individuals or anyone who voluntarily chooses vaccination.
Federal officials emphasized that this decision is based on updated scientific assessments and international trends. Dr. Makary stated that there is no current evidence showing a benefit for healthy kids, echoing the approach many countries have already adopted. Dr. Bhattacharya described the change as “common sense and good science,” pointing to the need for U.S. health policy to reflect real-time data rather than sticking to outdated pandemic-era guidelines. Both officials underscored the importance of tailoring vaccine guidance to actual risk rather than using a one-size-fits-all approach.
Critics of the earlier policy, including Secretary Kennedy, argued that recommendations for repeated COVID boosters in children lacked sufficient clinical backing. “Last year, the Biden administration urged healthy children to get yet another COVID shot, despite the lack of any clinical data,” he said. The revised guidance signals a broader reevaluation of public health messaging and acknowledges concerns raised by parents, clinicians, and researchers about overreach and medical necessity. According to Kennedy, this is part of a broader effort to reestablish trust in public health by aligning recommendations with credible evidence and prioritizing informed choice.
Scientific Basis Behind the Policy Change
The updated guidance reflects a growing body of evidence showing that healthy children and pregnant women without pre-existing conditions face a very low risk of severe illness from COVID-19. According to multiple studies conducted over the last two years, hospitalization and death rates in these groups have remained consistently low, especially with the currently circulating variants. As the virus has evolved and population-level immunity has increased through prior infection and vaccination, the original rationale for mass immunization in low-risk groups has weakened. Dr. Makary noted that “most countries have stopped recommending it for children,” underscoring a global pivot away from blanket vaccination strategies toward more targeted approaches.
What changed, according to officials, wasn’t just the virus—it’s the weight of new clinical data and international comparisons. Countries like the United Kingdom, Sweden, and Denmark have already revised or paused their pediatric COVID vaccine recommendations based on similar risk-benefit analyses. Their public health agencies have cited a lack of clear benefit for healthy children and concerns over rare but possible side effects such as myocarditis. U.S. officials now appear to be following that lead, suggesting that maintaining outdated vaccine guidance without current evidence creates confusion and may undermine trust in public health institutions.
Another key factor in the decision was the absence of long-term data supporting repeated COVID boosters in children and healthy pregnant women. The earlier push for additional doses was based largely on short-term antibody responses rather than clinical outcomes. Critics, including Dr. Bhattacharya, have argued that this approach failed to meet the standard of evidence typically required for routine vaccine recommendations. By removing the COVID vaccine from the schedule for these low-risk groups, federal agencies are effectively acknowledging the need for stricter thresholds when deciding which vaccines should be universally recommended, particularly for populations where the risk of severe disease is minimal.
What This Update Means for School, Travel, and Routine Care
With the COVID-19 vaccine no longer recommended for healthy children and pregnant women, many parents and expecting mothers may wonder how this affects things like school enrollment, travel plans, or routine healthcare. First, the CDC’s immunization schedule serves as guidance for physicians and school systems, but it doesn’t automatically change local vaccine requirements. School entry rules are set at the state or district level, so it’s important to check with your child’s school or local health department to see if COVID vaccination is still listed as required or optional. In many areas, COVID-19 was never made a mandatory school vaccine, and this federal change may prompt more districts to drop it officially.
If you’re planning travel—especially international—it’s also worth checking the destination country’s current entry rules. Some countries still ask for proof of COVID vaccination, while others have dropped all restrictions. For pregnant women and families with infants, this update may offer some relief from pressure to vaccinate before travel, but decisions should still be based on destination-specific risks and personal health history. If you’re visiting someone immunocompromised or entering a healthcare facility abroad, it’s still worth asking your provider whether temporary precautions or documentation might be helpful.
In terms of routine pediatric and prenatal care, this change may make appointments more focused and personalized. Without the push for universal COVID boosters, doctors may now have more time to review a child’s or pregnancy’s full health profile and tailor vaccine discussions accordingly. Parents can use upcoming well-child visits to double-check other key immunizations and ask specific questions about COVID-19 if they still have concerns. This is also an opportunity to clarify with your provider what’s now considered optional versus recommended based on your family’s health—not broad public policy. In short, the update simplifies the landscape but doesn’t remove the need for personal decision-making.
What Parents and Expecting Mothers Should Know and Do Now
If you’re a parent or expecting mother wondering what this change means for you, the key takeaway is this: the COVID-19 vaccine is still available, but it’s no longer routinely recommended for healthy children or pregnant women without underlying conditions. That doesn’t mean you should ignore the topic—it means the decision is now more personal. Talk to your pediatrician or OB-GYN about your specific situation, especially if your child or pregnancy involves any health risks like asthma, diabetes, or immune system issues. Doctors can help you weigh the current risks of COVID-19 against the benefits of vaccination based on the latest data, not outdated pandemic messaging.
For healthy families, this is a chance to reset and take a fresh look at your child’s vaccination schedule without the pressure of automatic COVID boosters. Focus on maintaining routine vaccines that have decades of proven benefit—measles, polio, tetanus, and others. At the same time, continue basic preventive steps that still make sense: stay home when sick, practice good hand hygiene, and keep up with checkups. If your child or household is exposed to someone with COVID, there’s still no harm in discussing temporary precautions with your doctor, especially for vulnerable family members like grandparents or those with chronic illnesses.
Pregnant women without health issues can also shift their attention to other important aspects of prenatal care. Vaccines like Tdap and flu remain recommended during pregnancy to protect both mother and baby. If you’re unsure about how COVID fits into the picture now, ask your doctor to walk you through the risk in practical terms. For some women, the COVID vaccine may still be reasonable depending on timing and exposure risk, but it’s no longer considered routine for all. This change is about putting decision-making back in your hands with your healthcare provider—not following one-size-fits-all mandates. The more informed you are, the better positioned you’ll be to make decisions that match your family’s actual needs.



